Are you a HIPAA covered entity? That’s the question you need to answer before building any compliance strategy or handling patient health data securely.
Due to high healthcare data breaches and stricter enforcement policies, a small misclassification can cost millions in fines, damage your reputation, and erode trust with partners.
Most companies misunderstand the definition of a covered entity under HIPAA, leaving themselves exposed. Incorrect assumptions often create compliance traps that surface when it is already too late.
This guide gives you a step-by-step path to clarity. You’ll learn what a covered entity under HIPAA means, what is exempted, where risks hide, and how to avoid costly mistakes.
Quick Summary:
Now, let’s begin by looking at each of them in detail, starting with understanding HIPAA itself and exploring the covered entities.
What is a Covered Entity Under HIPAA?
HIPAA (Health Insurance Portability and Accountability Act) was introduced in 1996 to standardize healthcare data, improve insurance portability, and protect health information. Over time, it became a standard of compliance for healthcare-related organizations.
Its main purpose is simple: safeguard protected health information (PHI). PHI includes patient names, addresses, Social Security numbers, medical records, and anything tied to an individual’s health or payment data.
The entities that electronically transmit protected health information (PHI) in standard transactions are required to comply with the HIPAA rules and are called the covered entities.
HIPAA does not cover every entity touching health data. Instead, it applies only to covered entities under HIPAA and their business associates who handle the PHI.
Three key rules form the framework, and each of them imposes distinct duties on covered entities and business associates.
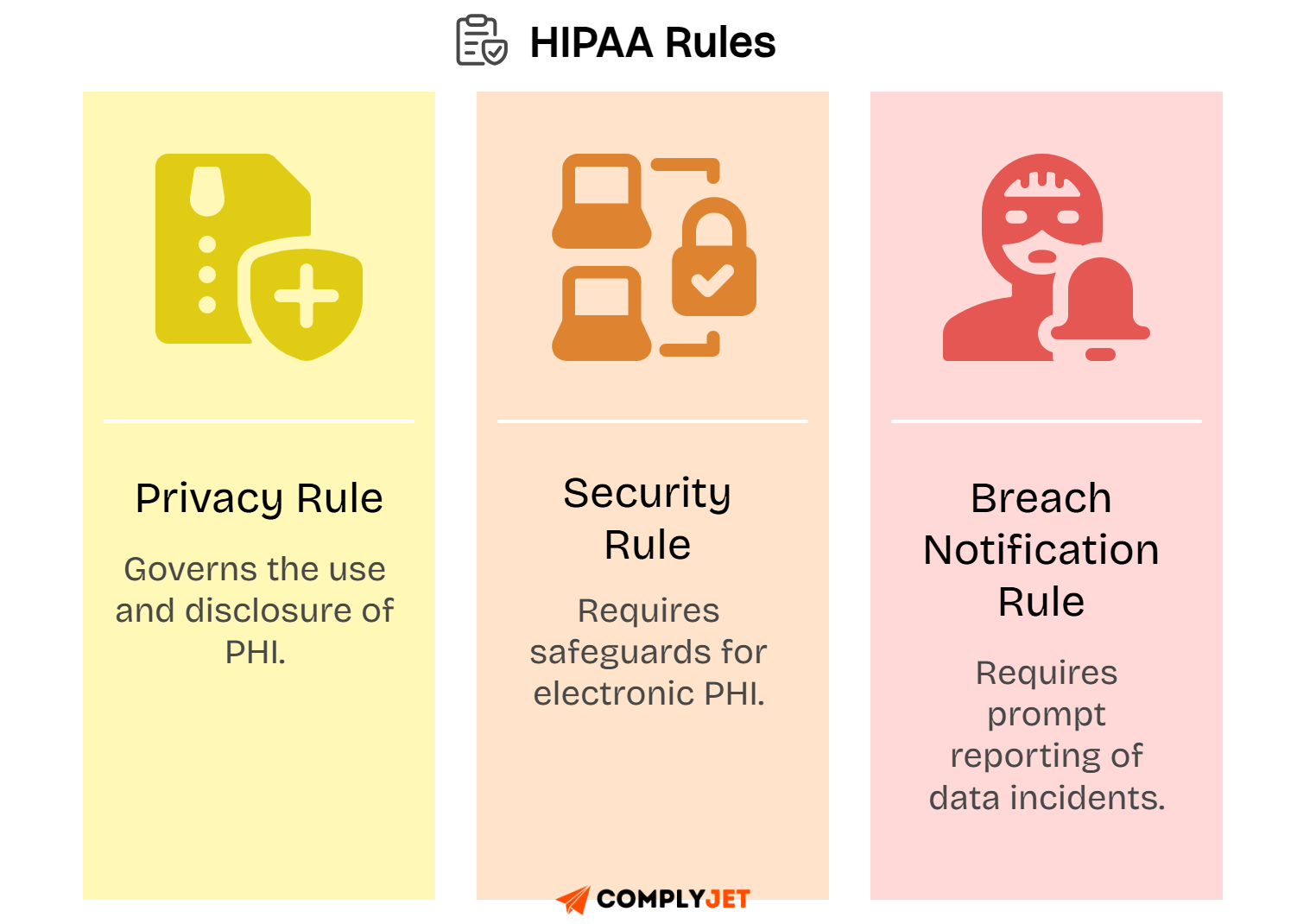
Understanding these three rules is essential because every HIPAA compliance program is built on them. Together, they define how covered entities must operate securely and in compliance with the law.
With the foundation set, the next step is to explore the categories of covered entities HIPAA regulates.
What are the Categories of Covered Entities?
Covered entities under HIPAA fall into three main categories. Each plays a unique role in handling health information and must meet compliance requirements.
Health Plans
A health plan is any individual or group program that provides or pays for health care services. This includes insurance companies and government-administered programs.
Examples of HIPAA covered entities in this category are health insurance companies, employer-sponsored plans, Medicare, Medicaid, CHIP, and veterans & military health programs.
Small or self-funded employer health plans may escape HIPAA if they cover fewer than 50 participants and are fully self-administered without third-party vendors, but once they outsource claims processing, they come under HIPAA covered entities.
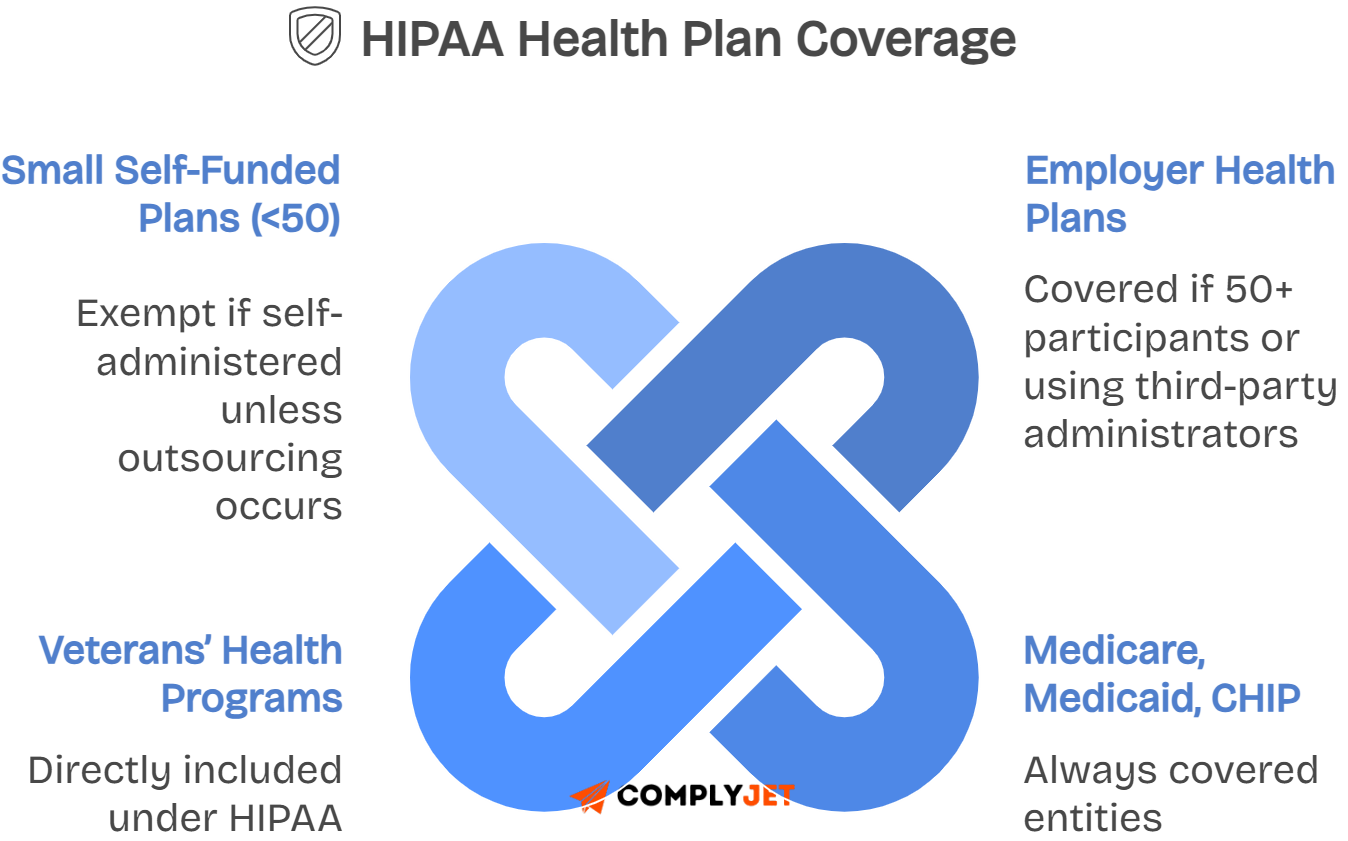
Understanding whether your company's health plan is a covered entity under HIPAA is essential before moving to providers that directly deliver care.
Healthcare Providers
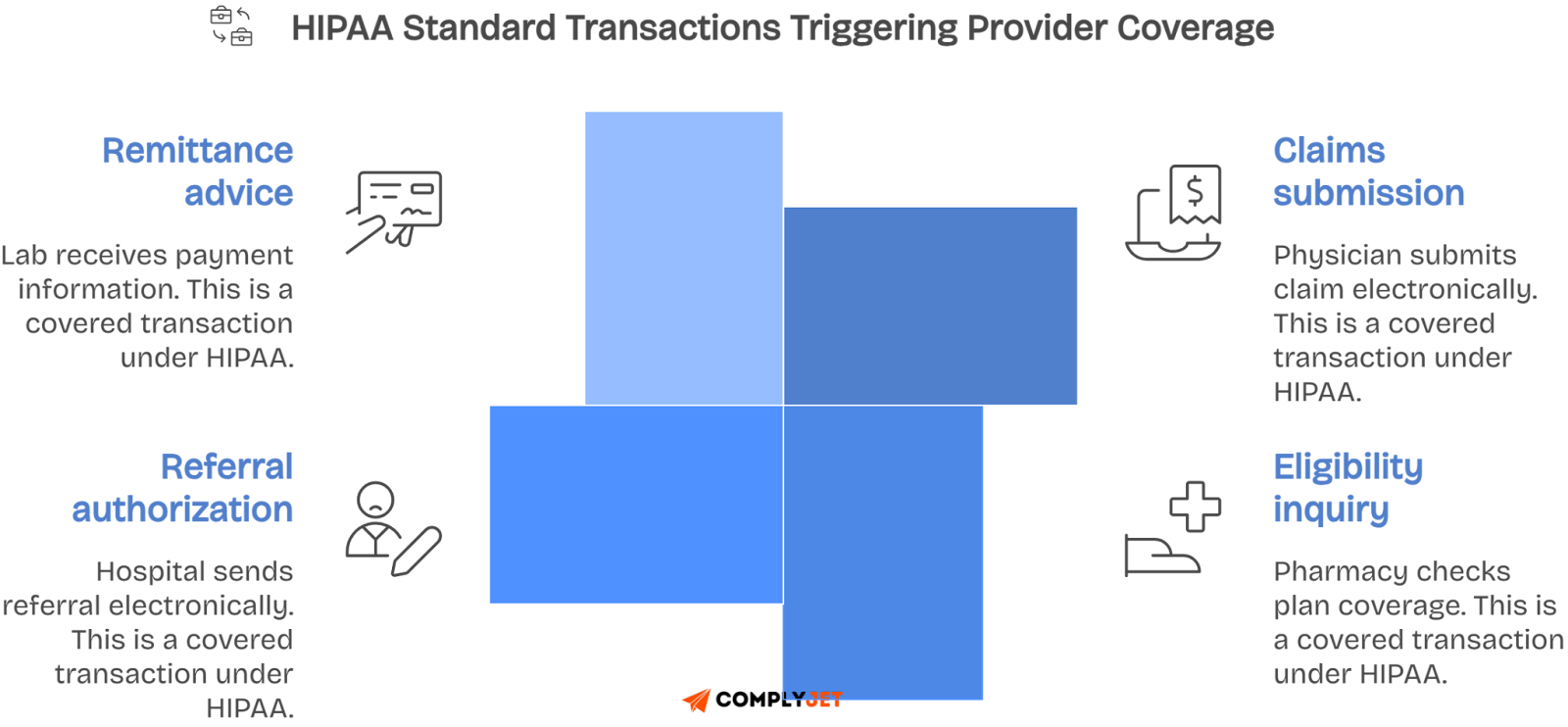
Healthcare providers include doctors, dentists, pharmacies, laboratories, therapists, and psychologists. They qualify as HIPAA covered entities when transmitting PHI electronically.
They qualify as covered entities if they furnish services and transmit PHI electronically in standard HIPAA transactions like claims, eligibility checks, or referrals.
A paper-only medical practice with no electronic claims is not a covered entity, while an EHR-enabled clinic transmitting PHI electronically is.
A common trap is outsourcing billing to a vendor. Even if a vendor submits electronic claims, the healthcare provider remains a covered entity under HIPAA.
Identifying providers as covered entities clarifies compliance duties, setting the stage for organizations that process PHI without delivering direct care.
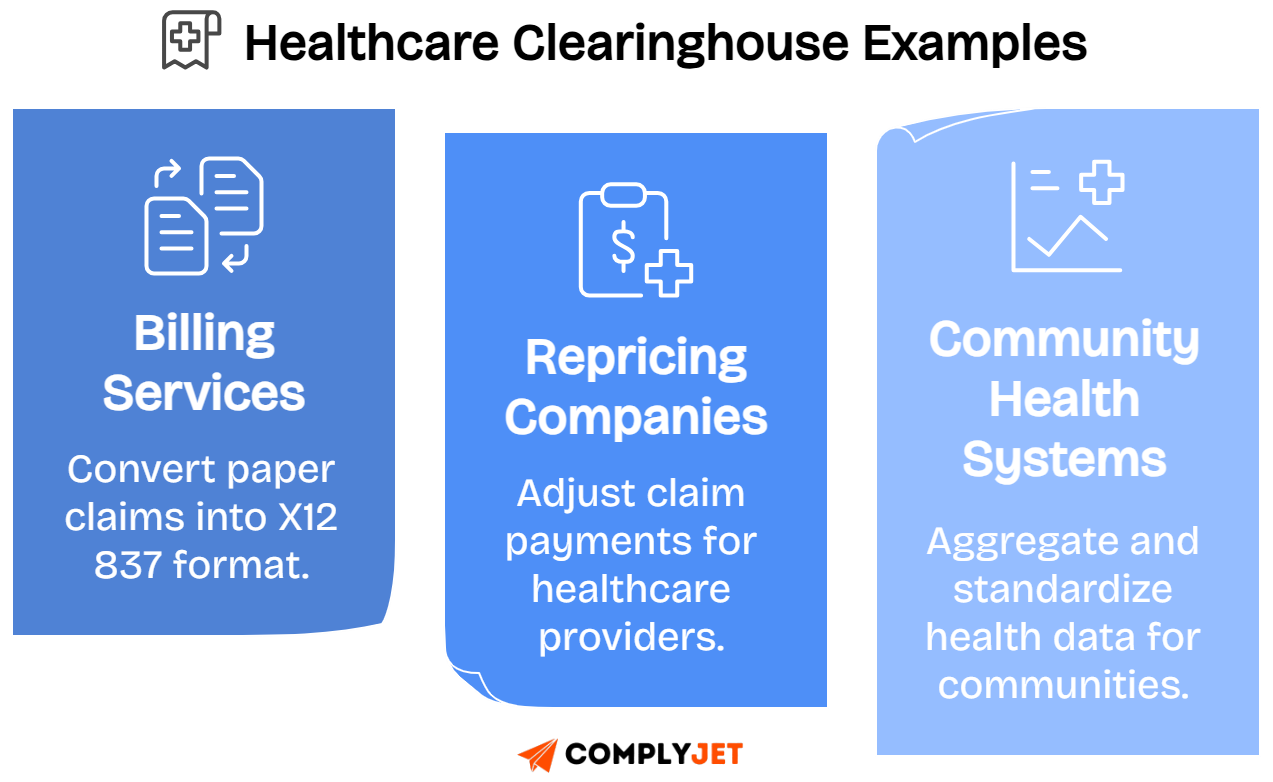
Healthcare Clearinghouses
Healthcare clearinghouses process or convert non-standard health data into HIPAA-standard transactions and formats, enabling smooth information exchange between plans and providers.
Examples include billing services, repricing companies, and community health information systems that standardize or translate data for health plans and providers.
Unlike business associates, clearinghouses are directly liable under HIPAA for safeguarding protected health information and ensuring compliance with privacy and security rules.
Recognizing clearinghouses as covered entities completes the core definition, allowing us to next explore the role of business associates in compliance.
Role of Business Associates
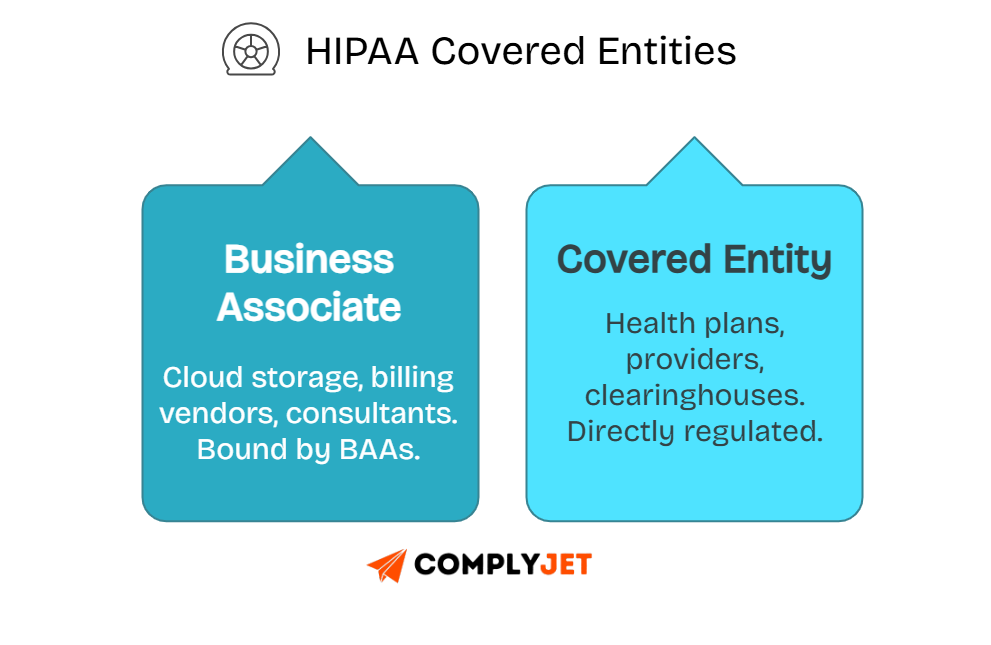
Business associates under HIPAA play a critical role by supporting covered entities while directly handling protected health information. Their responsibilities are clearly defined and strictly enforced.
Definition and Examples
A business associate is any third party that creates, receives, or transmits PHI for a covered entity under HIPAA.
Examples include cloud providers hosting medical data, consultants performing audits, transcriptionists converting clinical notes, and software vendors processing electronic claims.
The distinction is clear: a covered entity provides or pays for healthcare, while a business associate supports them by enabling compliant PHI management.
Understanding these roles matters, as business associates face direct HIPAA enforcement just like covered entities, shaping contracts and accountability across your vendors.
Responsibilities Under HIPAA
First, execute a Business Associate Agreement (BAA) before engaging any vendor that handles PHI on your behalf. This contract defines responsibilities.
Next, meet HIPAA Security Rule requirements by implementing technical, administrative, and physical safeguards to protect electronic PHI at every step.
Business associates must also notify covered entities promptly of any data breach, enabling compliance with strict HIPAA breach notification timelines.
These responsibilities make due diligence essential when selecting vendors, setting the stage for understanding HIPAA’s wider regulatory framework.
Regulatory Framework
HIPAA establishes clear rules that covered entities and business associates must follow, creating a shared compliance baseline for handling health information.
The Privacy Rule governs how PHI can be used and disclosed across treatment, payment, and operations.
The Security Rule defines safeguards for protecting electronic PHI, covering administrative, technical, and physical measures.
The Breach Notification Rule requires timely reporting of PHI breaches to individuals, regulators, and sometimes the media, depending on the scope.
Together, these rules define the heart of HIPAA compliance and directly guide how organizations structure their internal policies.
Administrative Requirements
Covered entities and business associates must designate HIPAA privacy and security officers to oversee compliance efforts and internal accountability.
You must also implement documented policies, covering PHI handling, data security, and workforce responsibilities for compliance.
Training programs are mandatory, ensuring staff understand their role in protecting PHI and following HIPAA requirements in practice.
These administrative safeguards create governance structures that support daily compliance, linking directly to permitted PHI uses and disclosures.
Permitted Uses and Disclosures
HIPAA allows PHI use for treatment, payment, and healthcare operations without patient authorization. These are the core permitted functions.
Exceptions exist for public interest, including disclosures to law enforcement, public health, and oversight agencies when legally required.
Incidental disclosures, like overheard conversations in a clinical setting, are permissible if safeguards are applied.
These rules highlight the need to restrict PHI access, which leads to the minimum necessary standard.
Minimum Necessary Standard
HIPAA requires you to limit PHI use and disclosure to the smallest necessary amount for any purpose.
For example, an insurance clerk should access billing codes, not entire medical histories, when processing a claim.
Non-compliant cases include sharing full patient files when only limited details are needed for operational tasks.
Applying this standard effectively reduces risk exposure and strengthens overall compliance posture.
How Important is Being HIPAA Compliant?
Understanding why HIPAA compliance matters helps you weigh risks and opportunities. Non-compliance damages trust, while adherence builds credibility and long-term resilience.
Risks of Non-Compliance
Civil penalties can reach $1.9 million per year for repeated HIPAA violations, creating significant financial strain on smaller organizations.
Criminal penalties include fines and possible imprisonment when PHI is misused knowingly, adding legal and reputational damage beyond civil enforcement.
The HHS Office for Civil Rights (OCR) actively enforces HIPAA, with past cases resulting in multi-million dollar settlements for improper PHI disclosures.
These risks highlight why compliance is essential, paving the way to consider the benefits of following HIPAA guidelines.
Benefits of Adhering to HIPAA Guidelines
Protecting patient trust is the most valuable outcome, as patients expect their personal health data to remain secure and confidential.
Avoiding breaches prevents lawsuits and costly investigations, saving you time, legal expenses, and reputational harm that is hard to repair.
Compliance also enables enterprise partnerships, as larger healthcare organizations require HIPAA alignment before collaborating or exchanging patient data.
These benefits show compliance as a growth enabler, guiding the transition into comparing covered entities with business associates.
Covered Entities vs Business Associates
Covered entities and business associates share responsibilities under HIPAA, but differ in how obligations are applied and enforced.
Legal Distinctions
Covered entities like providers, health plans, and clearinghouses are directly regulated under HIPAA’s Privacy, Security, and Breach Notification Rules.
Business associates are regulated contractually, through Business Associate Agreements, but still face statutory enforcement after the HITECH Act expansion.
Covered entities act as principals under HIPAA, while business associates act as agents, creating layered but distinct compliance requirements.
These distinctions create overlap in responsibilities, which becomes clearer when examining duties shared by both groups.
Overlapping Duties and Responsibilities
Both covered entities and business associates must implement HIPAA security safeguards, protecting PHI with technical, physical, and administrative controls.
Both are subject to breach notification requirements, ensuring individuals and HHS are informed when PHI is improperly accessed or disclosed.
Covered entities must also execute BAAs with all business associates, binding them contractually to HIPAA rules and extending liability downstream.
These overlapping duties ensure accountability throughout the ecosystem, preparing you to explore how state laws interact with federal HIPAA requirements.
Covered Entities vs Business Associates at a Glance:
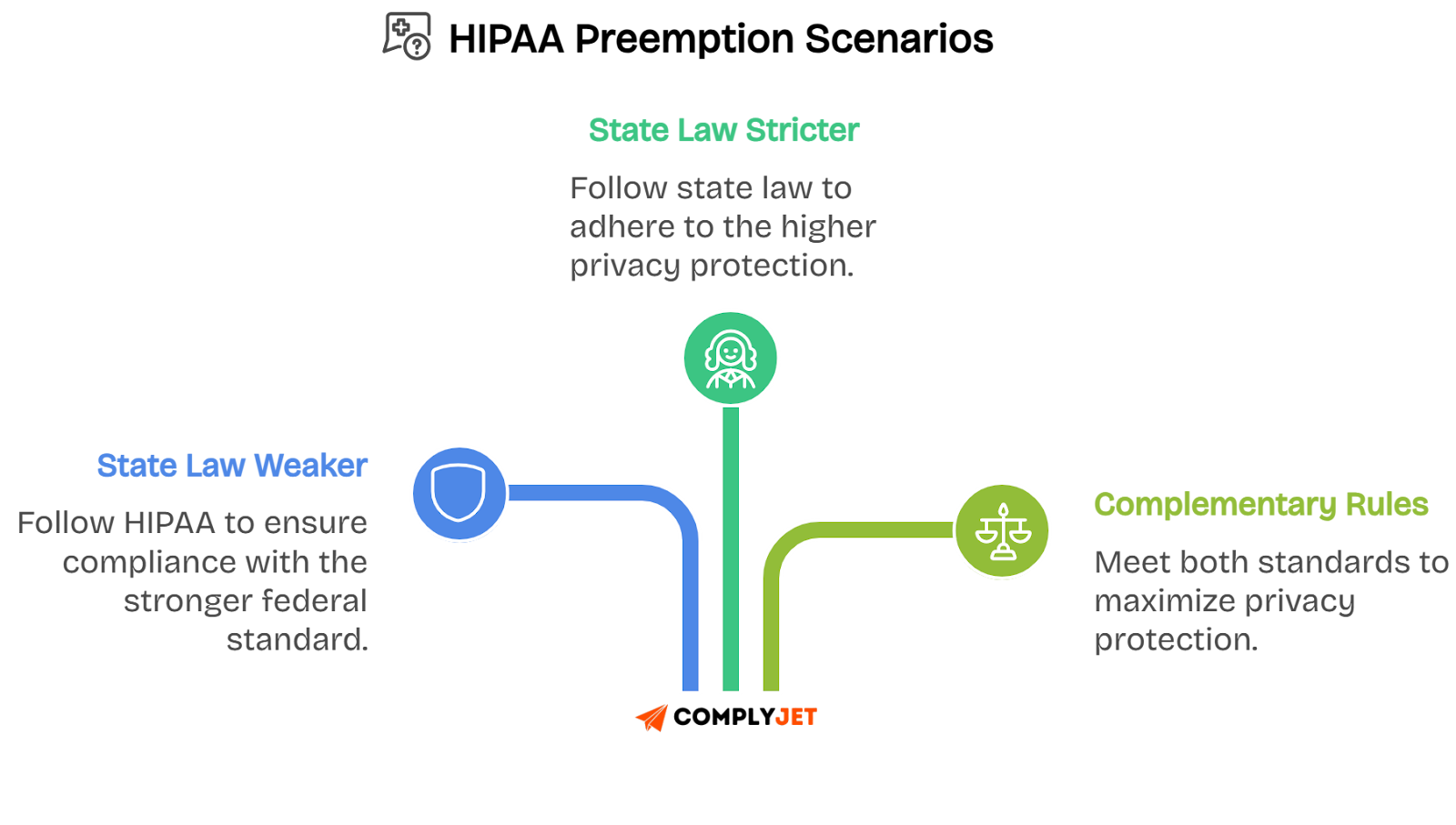
How State Laws Impact HIPAA Covered Entities?
State laws influence HIPAA compliance, sometimes creating stricter requirements that you must follow alongside federal rules. Knowing where they apply keeps you aligned.
Variations Across States
California’s CCPA and CPRA add rights for consumers, including data access and deletion, which go beyond HIPAA’s existing protections for patient information.
New York’s SHIELD Act requires specific safeguards for electronic health data, adding security measures even where HIPAA standards already apply.
When state law is stricter than HIPAA, you must follow the stricter requirement, ensuring compliance in both jurisdictions.
These differences highlight why monitoring state laws is essential before exploring how HIPAA’s preemption works.

Preemption by Federal Law
HIPAA generally overrides state laws that conflict, ensuring national consistency in how protected health information is managed.
However, HIPAA allows state laws that are stricter or complementary to stand, especially if they provide stronger patient protections.
For example, stricter consent requirements or shorter breach notification timelines in some states must still be followed by covered entities.
This interaction shows why compliance is multi-layered, preparing you to examine which entities HIPAA does not regulate.
Entities Not Classified as Covered Entities
Employers are not HIPAA covered entities, except when operating employer health plans subject to HIPAA’s rules.
Workers’ compensation carriers fall outside HIPAA, but must meet state-level confidentiality requirements when handling medical claims.
Life insurers, schools under FERPA, and law enforcement agencies also remain outside HIPAA’s definition of covered entities.
Knowing these exclusions clarifies obligations before considering special cases like self-funded plans and hybrid entities.
Special Cases and Situational Exemptions
Self-administered employer health plans with fewer than 50 participants are exempt from HIPAA requirements.
Plans covering only excepted benefits, like dental or vision, also escape HIPAA unless paired with broader health coverage.
Hybrid entities, such as universities with medical centers, can designate covered and non-covered functions separately, limiting HIPAA scope.
These exemptions demonstrate HIPAA’s narrow application, leading naturally into practical steps for determining covered entity status.
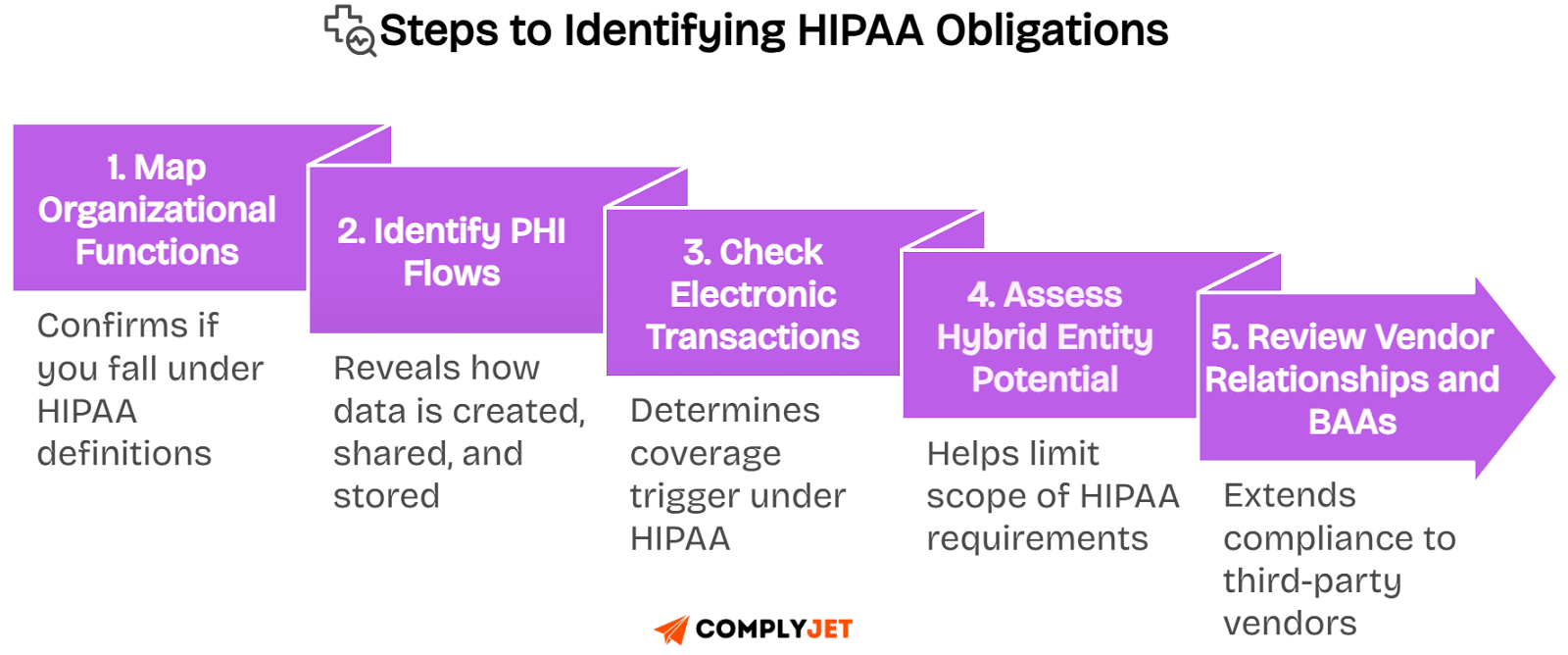
Practical Tips for Determining Covered Entity Status
Determining if you are a HIPAA covered entity requires a structured process.
Following a structured process makes it easier to determine if you qualify as a HIPAA covered entity and what compliance duties apply.
Step 1: Map organizational functions
Start by reviewing your business activities. List healthcare services, insurance roles, or data processing tasks that may bring you under HIPAA.
Step 2: Identify PHI flows
Next, track how protected health information moves through your systems. Note where it is created, transmitted, or stored, including third-party involvement.
Step 3: Check electronic transactions
Confirm if you conduct HIPAA-standard electronic transactions, such as billing claims or eligibility checks. Even one transaction can trigger covered entity status.
Step 4: Assess hybrid entity potential
Evaluate if your organization mixes healthcare and non-healthcare functions. Consider designating healthcare components to limit HIPAA’s scope to relevant areas.
Step 5: Review vendor relationships and BAAs
Finally, analyze vendor roles. Ensure Business Associate Agreements are signed with all third parties handling PHI on your behalf.
Resources for Clarification and Assistance
You don’t need to guess your HIPAA status. Several resources make the process straightforward and reduce uncertainty around compliance obligations.
The HHS Covered Entities Decision Tool provides a step-by-step questionnaire, helping you determine if you meet the HIPAA definition of a covered entity.
The CMS “Are You a Covered Entity?” guide offers plain-language explanations and examples, making it easier to apply rules to your organization.
OCR FAQs and enforcement examples highlight how regulators interpret HIPAA in practice, showing what mistakes to avoid and how penalties are applied.
Compliance automation platforms like ComplyJet help you go beyond one-time checks by offering continuous monitoring, BAA management, and audit-ready documentation.
Automation in HIPAA Compliance
Automation simplifies HIPAA compliance by replacing manual work with efficient, repeatable systems that save you time and reduce risk exposure.
Start with automation tools that manage HIPAA controls for you. These platforms centralize evidence, policies, and PHI safeguards, ensuring consistency.
Use continuous monitoring features to track PHI security across systems. This helps identify risks quickly and keeps you aligned with HIPAA requirements.
Automated policy management and workforce training modules ensure staff stay informed, while audit-ready evidence collection reduces preparation stress for external reviews.
Platforms like ComplyJet give startups and enterprises a cost-effective way to stay compliant, combining automation with structured documentation and real-time alerts.

FAQs
Here are detailed answers to common questions about HIPAA covered entities, designed to clear confusion and give you direct, actionable clarity.
What are the examples of a covered entity?
The examples of a covered entity include Medicare, Medicaid, insurance carriers, hospitals, physicians, pharmacies, and billing clearinghouses that manage electronic healthcare transactions.
Are police covered entities under HIPAA?
No, police are not HIPAA covered entities. However, they may access PHI under legal exceptions, such as court orders or public safety requirements.
What entities would not be regulated by HIPAA?
Entities like gyms, wellness apps, or financial institutions handling health-related data outside healthcare operations are not regulated by HIPAA. Employers, life insurers, schools governed by FERPA, and workers’ compensation carriers are also not covered entities under HIPAA.
What are the HIPAA standards that covered entities must follow?
They must follow privacy protections for PHI, security safeguards for ePHI, and breach notification requirements when unauthorized disclosures occur.
What is the difference between covered entities and business associates?
Covered entities provide or pay for healthcare, while business associates support them by handling PHI. Both are accountable but through different obligations.
How long must covered entities keep HIPAA records?
Covered entities must retain HIPAA documentation for at least six years from the date of creation or last effective date, whichever is later.
What happens if a covered entity violates HIPAA?
Violations can lead to fines up to $1.9 million per year, corrective action plans, and in severe cases, criminal penalties including imprisonment.
Conclusion
Determining if you are a HIPAA covered entity is the foundation of your compliance journey. It shapes every responsibility you carry under federal law.
Covered entities must follow the HIPAA Privacy Rule, Security Rule, and Breach Notification Rule, ensuring PHI is always protected and properly managed.
Misclassification creates hidden traps, exposing you to fines, reputational loss, and operational risk. Taking time to define your role prevents costly mistakes.
Adopt structured compliance processes, use automation tools like ComplyJet, which offers HIPAA Compliance Automation for $4999/year to protect patient trust while keeping your organization secure and audit-ready.
Start Our Free Trial Now!
.png)